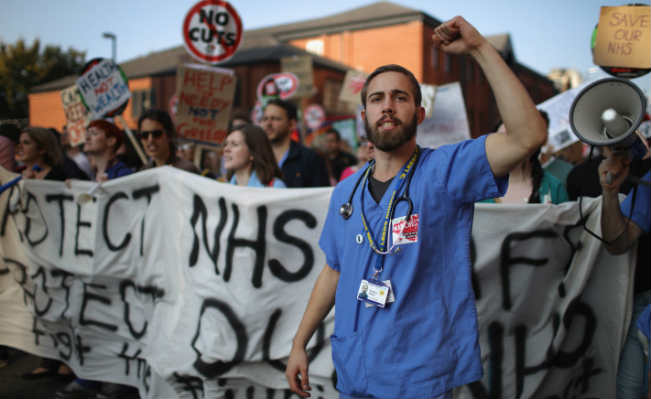
 Junior doctors protesting outside the Tory party conference in Manchester. Image: Getty
Junior doctors protesting outside the Tory party conference in Manchester. Image: Getty
With an unprecedented 98% of junior doctors voting in favour of strike action, Mona Kamal considers how they joined the frontline in defending the NHS
For the first time in 40 years, the union for doctors, the British Medical Association (BMA) balloted its members for industrial action. Junior doctors responded by voting overwhelmingly to enable a rolling programme of strikes, including two full days of walkouts. The strikes, which begin next week, are in response to proposed contract changes that are unsafe for patients – because of the removal of safeguards that protect doctors from working dangerously long hours, and also unfair fornon-consultant grade doctors, like me,who will seea 20-30% reduction in pay.
The pay cut will be implemented by redefining what constitutes “unsocial hours”. The plan is to extend the normal working week to include 7am to 10pm, Monday to Saturday, with these additional hours paid at the lower basic rate. This comes in addition to loss of pay protection for those choosing to take time out, including maternity leave, thus widening the gender pay gap.
98% of doctors voted in favour of strikes, weeks after thousands marched on Whitehall in angry protest. This is a remarkable show of unity and decisiveness from a group of people who by and large are not known for strident political activism, let alone open revolt. Jeremy Hunt likened junior doctors to “militants” but this could not be further from the truth. This is a group of professionals who are accustomed to making personal and financial sacrifices for the privilege of doing a job they love, but are rarely like to stick their heads above the parapet.
So why now? The BMA has said we need to “resist a contract that is bad for patients, bad for junior doctors and bad for the NHS” but there have been repeated assaults on the NHS that have failed to mobilise doctors or provoke this level of protest. Today’s junior doctors have witnessed the damage caused by Private Finance Initiatives, the deliberate underfunding by successive governments leaving services in crisis and the persistent smear campaigns to erode the public’s trust in the NHS.
Most notable is the Health and Social care Act of 2012, which effectively legislated for the dismantling of the NHS and opened the door for unlimited privatisation. Attacks on the NHS are not new, neither are the attacks on other healthcare professionals. But the deterioration is cumulative, and now cuts and privatisation are affecting junior doctors directly.
Speaking to junior doctor colleagues, there is an admission that despite an awareness of the issues, we were guilty of having our heads buried in the sand, and sadly it has taken an attack on our own working conditions and pay before we began to truly engage with wider questions around health policy.
But is this fair on junior doctors? I would argue that whilst this fight may have been triggered by pay cuts, it has been quick to evolve into so much more. It has succeeded in laying bare levels of anger about the destruction of the NHS that until now many of us were unsure existed; anger, it turns out, that most of us had been feeling, but in isolation. The proposed changes to our contracts suddenly made the fight more personal and gave us a starting point for channelling that discontent and creating platforms to begin voicing our concerns.
For me personally, this whole process has also exemplified the ways in which our ideas evolve, and the development of social consciousness originates from our own lived experience. An example of this might be the likely change in attitudes amongst some junior doctors towards the whole idea of industrial action. Although great care has been taken to avoid any disruption to services (something of an oxymoron when planning industrial action), there is nevertheless a lot of anxiety amongst doctors for whom this is all quite new territory – no doubt for some, personal barriers have had to be overcome to justify a full walk out.
Friends on social media, who months earlier had been less than sympathetic towards tube drivers during their strikes, were ready to embrace strike action themselves. This is particularly compelling when we consider that the RMT’s dispute around rebranding of anti-social hours to bring about 24-hour tubes (with no changes in staffing levels and little consideration of impact on health and safety) closely mirrors our own.
Confronting similar attacks on our own working conditions may have useful consequences. I think ultimately it will modify certain perceptions towards strike action, reframing it in our minds as a reasonable, even necessary course of action to take in order to safeguard basic rights, rather than one that is motivated by greed, as is often reported.
Crucially, it will also leave us considerably more attuned to threats to working people in other sectors, reinforcing a class consciousness and making collective action more feasible. As I write this, for example, the junior doctor forum on social media is dominated by anger about withdrawal of the NHS bursary for trainee nurses, with a call for even wider “solidarity strikes”.
So maybe we can be grateful to Jeremy Hunt for picking this fight. We have banded together effectively and grown in confidence, and it will take a lot for this generation of junior doctors to revert back to the sense of powerlessness and isolation that caused us to simply bury our heads in the sand. This campaign now needs to be broadened to include other NHS workers – there are over 1.5 million healthcare professionals employed by the NHS. How much more effective would we be if a threat to the working conditions of one group of NHS workers was rightly perceived as a threat to all, and we were not so fragmented into several individual unions?
The standard of care provided in our health service is made possible only by the effective teamwork and mutual support between different healthcare professionals: nurses, psychologists, occupational therapists and social workers, to name a few. It is time for the integrated approach we apply to individual patient care to be applied in safeguarding the future of the NHS.